This blog entry is not about my cancer. It’s focused on how genetic research and findings are transforming the field of cancer treatment. The first part of this blog will provide a foundation by way of definitions and a few basic premises. The second part will cite an article in today’s WSJ about how genetic testing could improve the prognosis and ultimately the treatment of prostate cancer.
Definitions, Foundation, and Hypothesis
==================================
Cancer cells: Uncontrolled growth of aberant cells in the body. Cancer cells can grow, divide, and invade normal tissue in the body.
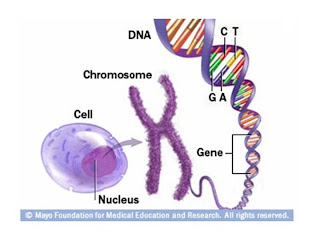
Gene: The basic unit of heredity in a living organism. All living things depend on genes. Genes hold the information to build and maintain an organism's cells and pass genetic traits to offspring. There are approximately three billion genes in humans.
DNA (deoxyribonucleic acid): A long linear polymer found in the nucleus of a cell and formed from nucleotides and shaped like a double helix; associated with the transmission of genetic information
Chromosome: An organized structure of DNA and protein that is found in cells. It is a single piece of coiled DNA containing many genes, regulatory elements and other nucleotide sequences. Chromosomes also contain DNA-bound proteins, which serve to package the DNA and control its functions. Humans have 22 chromosome pairs plus two sex chromosomes.
Genome: An understanding of the complete set of a living organism’s DNA.
Human Genome Project (HGP): An international scientific research project with a primary goal to determine the sequence of chemical base pairs which make up DNA and to identify and map the approximately 20,000–25,000 genes of the human genome from both a physical and functional standpoint.
Cancer Genome Project: Building off of the HGP and using high throughput mutation detection techniques, its goal is to identify somatically (i.e., cells in the human body) acquired sequence variants/mutations and hence identify genes critical in the development of human cancers.
Proteins serve many different functions within the chromosome and there are many different types of proteins. As such, I’m not going to define “protein” see (Wikipedia for a definition if interested). One function of a type of protein is cell division, either to encourage or discourage a cell from dividing. Proteins are complex and some proteins which regulate the growth of cancer cells have unique pathways. Admittedly, my knowledge here is weak and therefore should be treated as such. With this caveat, I’ll try to provide an example. In Head and Neck cancer, which for the most part is Squamous Cell Carcinoma, there is a protein called p53. This protein is also known as a tumor suppressor. There are other proteins which inactivate protein p53. Plus, to add to the complexity, the p53 protein may become compromised. So, in theory, if one could either 1) destroy the mutant p53 protein or 2) inactivate the proteins which inactivate the protein properly functioning p53 (yes, a double negative), then p53 could do its job in blocking the unregulated growth of cancer cells. From here, I’m on even thinner ice as I’m not sure about the relationship between p53 and my next statement (yet). Tarceva, a drug I have been on for 38 months is an EGFR (Epidural Growth Factor Receptor) inhibitor. It has special properties which in some way target a pathway into a protein which plays a significant role in solid cancer tumor growth. This is all very complex, so let me get to the hypothesis of this paragraph.
Hypothesis: If, through individualized genetic testing, one could find patients with an over-expression of the protein (or pathway) which Tarceva attacks, Tarceva (which is very expensive) could be targeted to those individuals for whom there is evidence of benefit (i.e., evidence based treatment). This in turn should increase the overall effectiveness of Tarceva on the population which is genetically receptive to this treatment regimen. It would in turn reduce unnecessary Tarceva treatment and reduce healthcare costs without impacting heath care effectiveness.
Today’s WSJ Article on Genetic Profiling and Cancer Treatment
============================================
You may have thought I forgot about part two of this blog entry. I found today’s (2/3/2011) news story in the WSJ titled, “New Clues to Treat Prostate Cancer,” fascinating. It is about how four genes play an intricate and interrelated role is predicting which individuals with prostate cancers have an aggressive cancer where treatment (e.g., radiation, surgery) is recommended versus one in which it should be watched without treatment.
Here are the article highlights. The findings so far is in mice, not man. Human testing is a few years off. One study cited in the article said that 48 men were treated with radiation or surgery to save one life. (Note, although this was not in the article, side effects from prostate treatment can include erectile dysfunction, incontinence, and surgical complications.) The article went on to say that if this genetic test could increase the odds of determining who should have treatment from our current standard of care test (an individual’s PSA level and biopsy) which predicts at a 60 – 70% to a 90% level that many men with a "favorable profile" might want to monitor the progress of their cancer for a while before deciding to undergo aggressive treatment.
To me, this is a game changer and yet another example of how our genetic understanding will impact medical practice over the coming years.
For those with access to the online version of the Wall Street Journal, here’s a link to the article…
http://online.wsj.com/article/SB10001424052748703960804576120194229203936.html?mod=djkeyword
Take care everyone.
Ed
Thursday, February 3, 2011
Subscribe to:
Posts (Atom)