Hi Out There!
4 years ago today my doctor suggested palliative care as a treatment option. Well, I'm still here. Some days that surprises even me. I'm 3 years and 2 months with no evidence of disease (NED) and my current status as of last December moved from NED to "clinical remission."
My sister sent me a book in early December titled, "The Emperor of All Maladies." It is a biography of cancer written by a cancer physician and researcher at Columbia University. It was published last month and was named as one of the 10 best books of 2010 by the New York Times Book Review Magazine yesterday. This blog entry reflects on information covered in that book; it is not a book review, but more about what I took away from it.
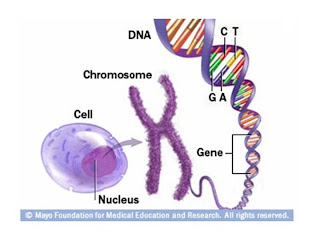
The book crystallized a concern which has been nagging at me for some time. The concern is that I am not cured and never will be. Cancer is a series of cell aberrations; it is not just one aberrant cell event. That is why one might hear the term precancerous; it is a cell (or group of cells) which are heading toward becoming cancer, but haven't fully matured. Some precancerous cells never mature, others do. Triggers for moving cells from one stage to another are becoming better understood due to genetic and genome research, but a single cell can lie dormant for decades just waiting for its trigger.
Recent studies support the hypothesis that some cancers are caused by cancer stem cells. By eliminating the body of all known active cancer cells via treatment and entering into a state of remission, cancer stem cells can still remain in one’s body. These unaffected and remaining cells can begin producing new aberrant cells leading to a relapse at any time. This insight, as well as others, is changing the way researchers view the "war on cancer" from one of curing it to one of treating it as a life long chronic illness. Although I am in remission, for me, this war is far from over and I relive it frequently.
The book also reinforced hope for the future by providing a much deeper understanding into the world of targeted cancer drug therapies. I’ve been on Tarceva, a targeted chemotherapy drug, for over 3 years. Two new, potentially more effective, targeted therapy drugs are in the pipeline: OncoVEXGM (about to launch a phase III trial) and REOLYSIN (currently in a phase III trial). Both of these drugs are for head and neck cancer (note, these specific drugs were not mentioned in the book, but I’ve been following their progress elsewhere).
Without complaining (why me), I’ve tried in this blog over the years to provide insight to the reader that explains why cancer is an atrocious disease and at times how cancer patients and survivors feel. There is an excerpt in the book which resonated with me that may help one not touched directly by this disease understand how patients experience cancer. It was written in an essay titled
A View from the Front Line, by Maggie Jencks.
Maggie was diagnosed with breast cancer in 1988. She was treated with a lumpectomy and then a mastectomy. For several years she considered herself cured, but five years later she relapsed with metastatic breast cancer to her organs and bones. Aggressive chemotherapy failed and she died in 1995. Her analogy to cancer begins with her being awoken up mid-flight on a jumbo jet and thrown out with a parachute into a foreign landscape without a map. Here’s her essay…
“There you are, the future patient, quietly progressing with other passengers toward a distant destination when, astonishingly (why me?) a large hole opens in the floor next to you. People in white coats appear, help you into your parachute and - no time to think - out you go.
You descend. You hit the ground… But where is the enemy? What is the enemy? What is it up to? … No road. No compass. No map. No training. Is there something you should know and don’t?
The white coats are far far away, strapping others into their parachutes. Occasionally they wave but, even if you ask them, they don’t know the answers. They are up there in the Jumbo, involved with parachutes, not map-making.”
Although written over 15 years ago, the image, for me, still captures the desolation and desperation of many cancer patients. Oncology researchers, obsessed with radical and aggressive therapies, were devising newer parachutes, but with no systemic maps of the quagmire to guide patients and doctors. This is less true today than in the mid 1990s, but more progress is beneficial.
I realize this is a long blog entry, but I would be remiss in not sharing with you some further highlights from the book. Here they are in no particular order.
- The profession of oncology got its start based on the observation of the effects of mustard gas in WW I. This seems highly ironic.
- Ether, the first anesthetic, was not in use until the late 1800s. Mastectomies have been documented back to 500 B.C. I think back to all those poor women.
- If we don’t kill the tumor, we kill the patient. This short simple statement reflects why cancer doctors and researchers take such an aggressive treatment approach. You may have to read it a few times to get its full meaning.
- The pap smear was named after George Papanicolaous, a Greek cytologist at Cornell University. He began human trials in the late 1920s. It wasn’t until 30 years later that his earlier discovery began to become a mainstream cancer prevention procedure. For most of his career, he was ridiculed and ignored by his peers as discovering a useless procedure. The ironies in the book abound.
- The cancer genome project is in progress and is focused on mapping every cancer gene in every type of cancer. When complete it is estimated to be 10,000 times the size of the human genome project.
- We are winning the war on cancer; it just so happens to be a very long and complicated march.
I’ll stop my highlights here, but there were dozens of others such as the effect politics, fund raising, the tobacco industry, dedicated researchers / physicians, care providers, patients, other diseases (e.g., polio and HIV) and cancer advocates have shaped where we are today in the war on cancer.
I'd like to take this opportunity to thank my friends, family, physicians, and researchers for their continued support and effort. It feels good to be celebrating my Cancerversary today.
Take care everyone and Happy Holidays.